COLUMN/ THE WRITE LINE Dr. Amitav Banerjee
Dr. Amitav Banerjee
October 1, 2022: The coronavirus pandemic, which is well into its second year, continues to throw surprises. The sprint has turned into a marathon. Experts, who once spoke with confidence while mapping out the battleplans early in the pandemic, lost their way once the marathon entered alien territory. Their disorientation got aggravated as the promised missiles – the coronavirus vaccines – failed to live up to expectations.
Early in the pandemic, populations of almost all countries, barring a few such as Sweden, Japan, and Belarus, implemented severe restrictive measures like lockdowns, and closure of schools and businesses to “flatten the curve,” and prevent the overwhelming of hospital services.
These unprecedented measures were expected to last a few weeks to break “the chain of transmission.” People complied to these harsh measures. The pandemic of panic in the era of social media platforms spread faster than the virus itself.
Governments around the world pushed the envelope further. Whatever restrictions were imposed for a few weeks got extended to several months, interrupted only intermittently. The hope of achieving zero-Covid levels with the arrival of vaccines developed by novel technology and hyped by media, along with high panic levels maintained by 24X7 TV news channels, mesmerized people into submission.
Vaccines were rolled out in late 2020. Countries such as Israel were lauded for quickly vaccinating their population. Others followed with equal speed, particularly the so-called developed countries.
The WHO (World Health Organization) kept calling for vaccine equity deploring the Western world for hoarding vaccines and going for boosters, depriving the Asian and African countries of much-needed vaccines. Paradoxically, the latter continued to do well without these vaccines!
The honeymoon is now over. Countries with adequate mass vaccination coverage are facing surges both in cases and deaths, the trends paradoxically higher than the pre-vaccination period. The following graphs based on data available in the public domain for Israel, Japan, Taiwan, and Australia illustrate the paradox (See figures 1-4).
Mass vaccinations do not seem to have any impact at the population level. Many countries, such as Indonesia, Malaysia, Sri Lanka, Singapore – mainly in Asia and Southeast Asia – experienced the same paradox after the vaccine’s roll-out.
While experts keep repeating that the vaccine prevents severe disease and deaths, the graphs show spike in deaths post-vaccination. A study published in European Journal of Epidemiology found that trends of Covid-19 did not correlate with the population-level vaccination coverage. The investigators compiled data from 68 countries and 2,947 American counties.
Figure 1: Trend of cases and deaths in Israel before and after mass vaccination

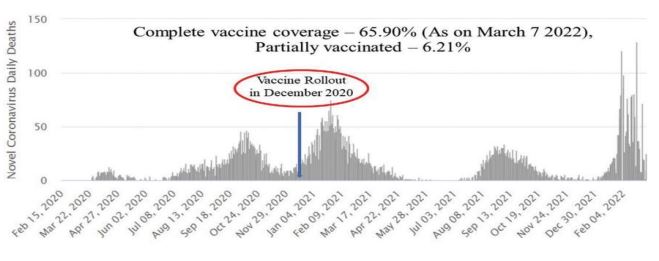
Figure 2: Trend of cases and deaths in Japan before and after vaccination


Figure 3: Trend in cases and deaths in Taiwan before and after vaccination

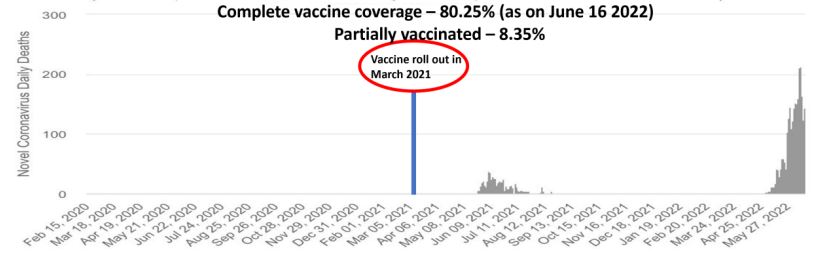
Figure 4: Trend in cases and deaths in Australia before and after vaccination


While these findings may seem paradoxical, a close look at India’s Covid-19 experience will help us understand the dynamics of the pandemic. India is a vast country with a population of over 1.4 billion. It has huge socioeconomic disparities. It has the richest as well as the poorest people in the world and in between all gradients of socioeconomic classes.
Covid-19 impacted different classes of people differently. Restrictive measures such as lockdowns and physical distancing, and business and school closures led to further “social distancing”. The poor became poorer but got faster and more robust herd immunity against the coronavirus disease; and the rich got richer but remained vulnerable and got fragile and uncertain vaccine-induced immunity.
Subsequent waves of the disease affected and continue to affect the middle and upper classes, but not the poor.
During the first wave, due to imitation of restrictive measures from the West, intense transmission resulted among the poor in their crowded living conditions in slums and tenements, while the middle-class and the affluent could shield themselves from the infection by working from home and observing all “Covid-appropriate behaviour.”
Mumbai’s Dharavi area, home to one of the biggest slums in the world with a population of a million, is the best example of this phenomenon. During the first wave, the residents of Dharavi acquired robust herd immunity without any vaccination. During successive waves, Dharavi was least affected whereas the middle-class and the affluent living in well-serviced and well-planned housing societies were most affected.
Subsequently, studies from across the world revealed that immunity acquired after recovery from natural infection is more robust and longer lasting compared to vaccine induced immunity. And with arrival of the Omicron variant of the virus and its subvariants, the graphs above suggest that the vaccine is hardly providing protection at the population level.
In June 2021, after the second wave, 67% of Indians had IgG antibodies, indicating they have encountered the virus and recovered resulting in robust immunity. As the antibodies levels fall after sometime but the immunity persists due to primed memory and T cells, the figure can be pegged at 80%.
A subsequent survey among children below 18 years of age in New Delhi in September 2021 revealed that 82% of them had IgG antibodies, before any vaccine roll-out among them. Similar finding were reported from many parts of the country.
It is also interesting to note that states in India such as Kerala, which did well to protect its people during the early phase of the pandemic, did badly later into the pandemic with surges in spite of the vaccine being available.
Around the world, the same pattern can be observed. Israel, Taiwan, Australia, New Zealand, Malaysia and other countries, which did well initially, are now experiencing surges in spite of high vaccination coverage, including two boosters.
The message from this phenomenon being played out in India mimicking the global experience is that one cannot prevent the natural course of a pandemic through human interventions, such as lockdowns, physical distancing, school and business closures, or through mass vaccination.
One can only postpone the inevitable. With dubious efficacy of mass vaccination, one should rework the cost-benefit analysis, which is an important aspect of health economics in public health practice.
It has relevance for India, which has the advantage of a large population base of young people who have already acquired robust herd immunity from natural infection. Chasing a rapidly mutating virus is like chasing a deer in the jungle.
Focused protection by vaccination of the elderly and the young with comorbidities on the advice of their personal physician rather than mass vaccination would be a prudent and cost-benefit approach.
The resources saved can be channelised to upgrade the vaccine to meet the challenge of new variants, and spend on our more pressing public health needs.
To put our public health problems in perspective: we lose over 2,000 children every day due to non-Covid illnesses against a background of malnutrition. Around 1,400, mostly young, die from tuberculosis daily. About 400-500, mostly young, get killed every day on Indian roads.
Besides, we have many unresolved health issues such as dengue, diarrhoea, typhoid, leptospirosis, etc. for which we haven’t yet developed a good reporting and monitoring system. These are our major public health problems.
Mindlessly imitating the West and dancing to their tunes will push these problems under the carpet, adversely impacting the health of our citizens.
REPUBLISHING TERMS:
All rights to this content are reserved. If you want to republish this content in any form, in part or in full, please contact us at writetoempirediaries@gmail.com.